Dott. Alberto Gobbi
Tra i migliori specialisti in Bio-ortopedia, Medicina Rigenerativa, Chirurgia Artroscopica e Medicina dello Sport IL DOTT. GOBBIPRENOTA UN CONSULTODott. Alberto Gobbi
Tra i migliori specialisti al mondo in Bio-ortopedia, Medicina dello Sport e Chirurgia Ortopedica
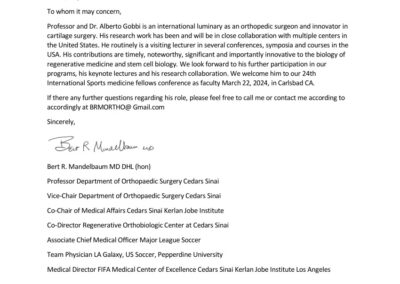
Chi è Alberto Gobbi
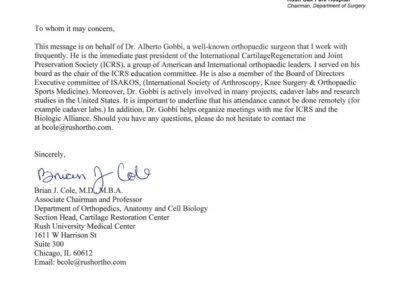
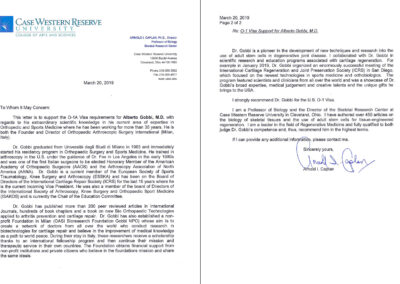
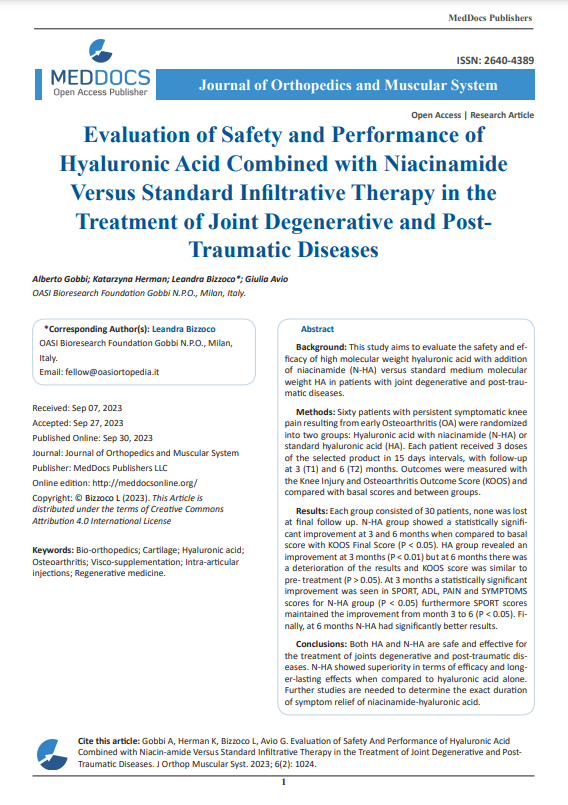
E’ stato tra i primi specialisti di ortopedia e medicina sportiva in Italia ad occuparsi di biotecnologie per il trattamento delle lesioni degli sportivi.
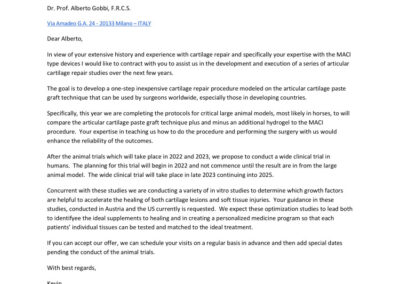
Da oltre 20 anni collabora con importanti centri di ricerca in Europa, Giappone e negli Stati Uniti alla sperimentazione di nuove bioterapie in campo ortopedico.
Chi è Alberto Gobbi
E’ stato tra i primi specialisti di ortopedia e medicina sportiva in Italia ad occuparsi di biotecnologie per il trattamento delle lesioni degli sportivi.
Da oltre 20 anni collabora con importanti centri di ricerca in Europa, Giappone e negli Stati Uniti alla sperimentazione di nuove bioterapie in campo ortopedico.
Prossima apertura
in Via Lamarmora 21, 20122 Milano
Come raggiungerci coi mezzi di trasporto?
Prenota un consulto
Hai bisogno di un parere per un problema ortopedico?
Pratichi sport ed hai subito un trauma?
Soffri di artrosi o problemi della cartilagine?
Da noi puoi trovare la soluzione!
Il Dottor Alberto Gobbi riceve su appuntamento negli studi medici O.A.S.I. di Milano, e Cento Cannoni di Alessandria, oppure fissa un consulto online per un parere!
Perche’ una persona dovrebbe cercare su Google una soluzione ai propri disturbi?
A cura del dr Kevin Stone ed Alberto Gobbi
Conosciamo pazienti ipocondriaci che ogni minimo mal di testa lo trasformano in una malattia potenzialmente mortale e talora anche contagiosa!
Questi soggetti non dovrebbero consultare Google ad ogni disturbo poiche’ sicuramente andrebbero a finire con lo stare peggio.
Questo non vale per tutti poiche’ in realta’ una persona attenta puo’ trovare molte risposte su internet e conoscere meglio il proprio problema.
Le Nostre Attività
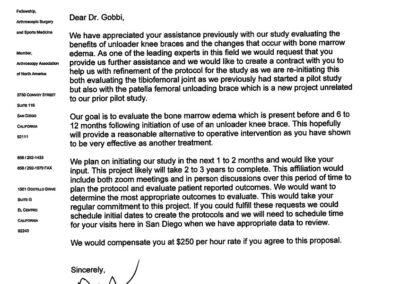
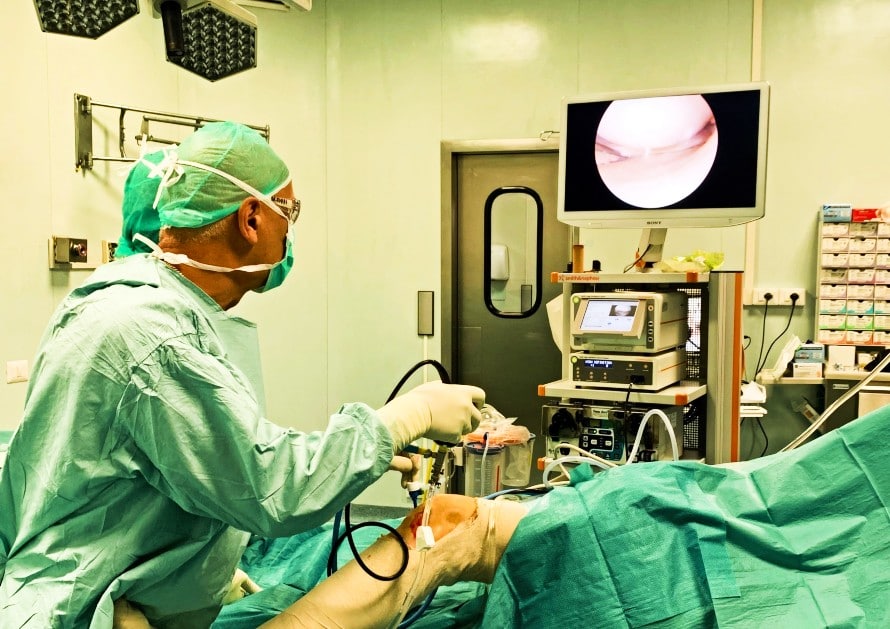
Il Dott. Gobbi ed il suo team Internazionale di specialisti offrono servizi avanzati ed innovativi di bio-ortopedia e medicina rigenerativa, chirurgia ortopedica, medicina dello sport.
Centro Internazionale di studio della cartilagine.
ANTI-AGING
BIO-ORTOPEDIA E MEDICINA RIGENERATIVA
MEDICINA DELLO SPORT
RIABILITAZIONE
Non perderti le nostre attività:
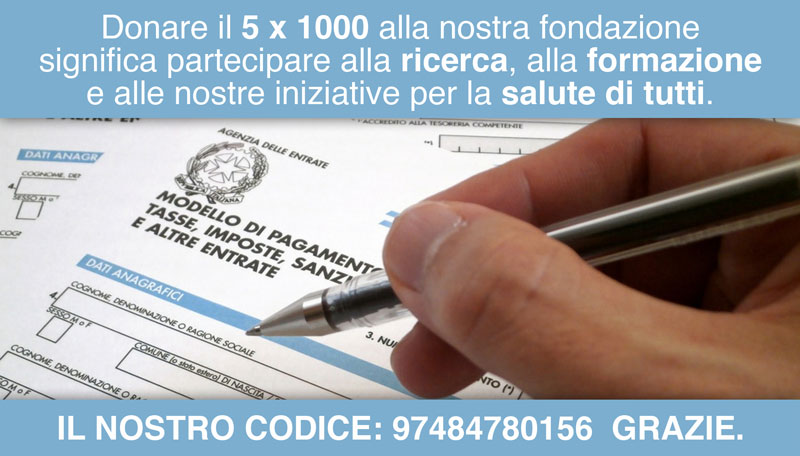
Dona il tuo 5 x 1000
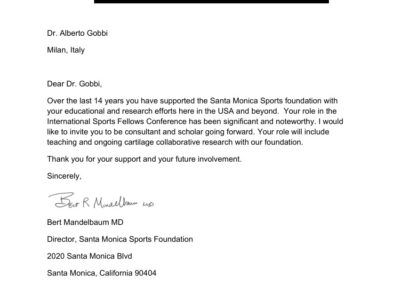
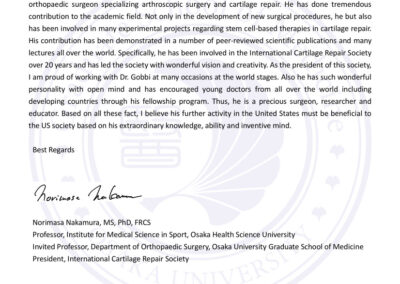
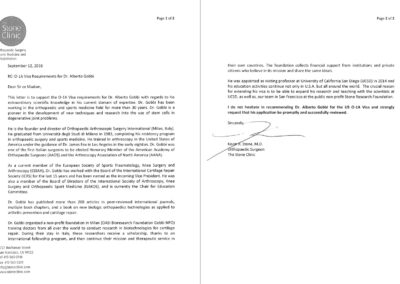
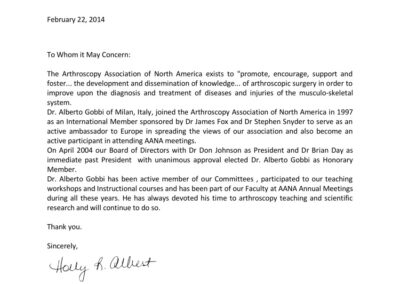
Cosa Dicono Di Noi
Il nostro obiettivo è farvi tornare alle attività che più vi piacciono!
Conosci La Tua Patologia
GINOCCHIO
ANCA
CAVIGLIA E PIEDE
GOMITO E POLSO
SPALLA
MALATTIE REUMATICHE E OSTEOPOROSI
COLONNA
ALTRE
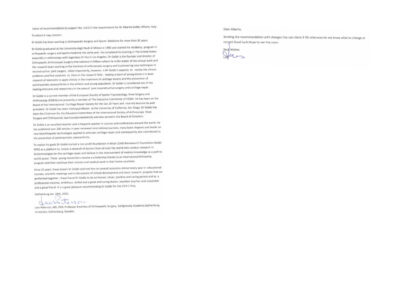
O.A.S.I. Bioresearch Foundation ONLUS
O.A.S.I. Bioresearch Foundation Gobbi Onlus è stata fondata nel 2007 dal Dott. Alberto Gobbi.
Lo scopo di questa Fondazione, senza fini di lucro, è aiutare giovani medici a ricercare nuove metodologie di prevenzione e cura delle patologie dell’apparato locomotore.
In 10 anni oltre 100 medici da più di 30 paesi del mondo hanno partecipato al programma di Fellowship Internazionale della Fondazione.